Opioids have a significant impact on the brain area that controls breathing. When taken in high doses, opioids can cause an overdose, characterized by a drastic slowing or complete cessation of breathing, which can be fatal. This critical effect on the respiratory system is what makes opioid overdose a serious medical emergency. Our opioid rehab in Atlanta, is here to help you or your loved one struggling with opioid addiction. Call us today to start your opioid addiction treatment.
What is an Opioid Overdose?
Opioid overdose is a critical health issue, primarily due to opioids’ ability to suppress the brain’s breathing regulation. Recognizing an opioid overdose involves noticing three key signs:
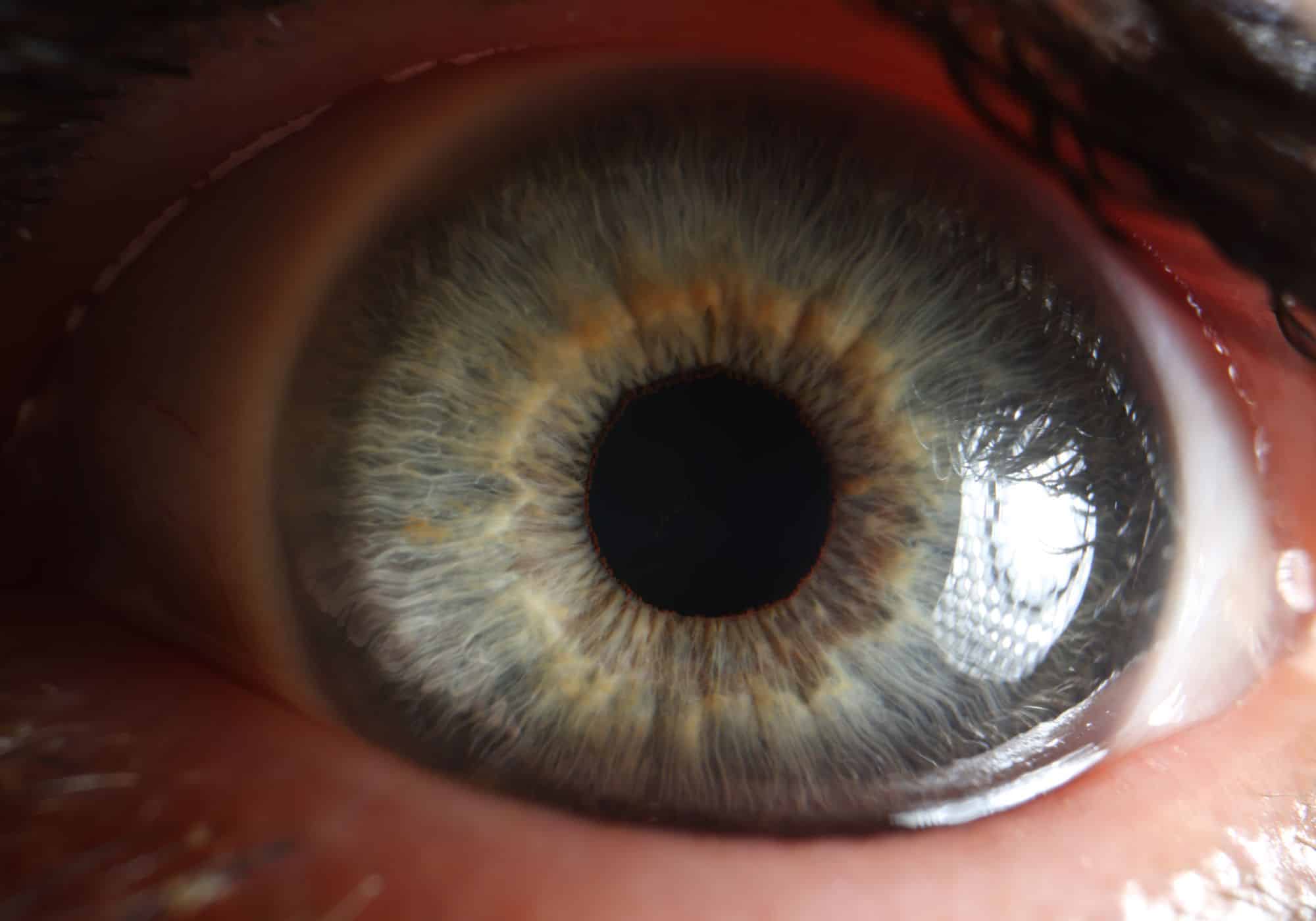
- Pinpoint pupils.
- Unconsciousness.
- Breathing difficulties.
In 2019, around 600,000 deaths globally were linked to drug use, with opioids accounting for nearly 80% of these. Notably, about 25% of these deaths were due to opioid overdose. The World Health Organization estimated that opioid overdoses caused approximately 125,000 deaths in 2019 alone. Non-fatal opioid overdoses occur much more frequently than fatal ones.
The incidence of opioid overdoses has been rising in several countries. This increase is partly attributed to the greater availability of opioids for chronic pain management and the emergence of highly potent opioids in the illicit drug market. In the United States, drug overdose deaths reached 70,630 in 2019, with about half involving synthetic opioids. From 2013 to 2019, the death rates from synthetic opioids in the U.S. soared by 1040%. The COVID-19 pandemic further exacerbated this issue, with a significant surge in drug overdose deaths, predominantly from synthetic opioids.
Fentanyl, a synthetic opioid around 50–100 times more potent than morphine, is used for pain relief and anesthesia. It’s listed on the WHO Model List of Essential Medicines. However, fentanyl and similar analogues like carfentanil, acetylfentanyl, butyrfentanyl, and furanyl fentanyl have been linked to a dramatic increase in opioid overdose deaths. Drug dealers often add fentanyl to other drugs like heroin or create counterfeit tablets resembling prescription medications, increasing the potency unknowingly to users. As a result, many individuals who test positive for fentanyl and its analogues are unaware they have consumed these substances.
What are the Signs of an Opioid Overdose?
Identifying an opioid overdose quickly is crucial, and there are several key signs to look out for:
- Pinpoint Pupils: The pupils become very small.
- Unresponsiveness: The person may fall asleep or lose consciousness and be unable to wake up.
- Breathing Difficulties: Breathing becomes slow and shallow.
- Choking Sounds: There may be choking or gurgling noises.
- Nausea and Vomiting: The person might vomit.
- Physical Weakness: The body may appear limp and unresponsive.
- Skin Changes: The skin can turn pale, blue, or feel cold to the touch.
- Weak Pulse: The heartbeat may be faint or hard to detect.
- Discoloration: Lips and fingernails might turn purple.
If you observe these signs in someone, it’s important to act immediately as an opioid overdose is a medical emergency.
What Causes an Opioid Overdose?
Opioid overdoses can occur under various circumstances, including:
- Recreational Use: Using opioids to achieve a high.
- Misuse of Prescription Opioids: Taking an extra dose or using a prescription opioid more frequently than prescribed, whether intentionally or accidentally.
- Combining Substances: Mixing opioids with other medications, illegal drugs, or alcohol can be particularly dangerous. This risk is heightened when opioids are combined with anxiety medications like Xanax or Valium.
- Taking Someone Else’s Medication: Using opioid medication prescribed for another person can lead to overdose. This is especially risky for children who might accidentally consume medication not intended for them.
- Medications for Opioid Use Disorder (MOUD): While MOUD is a treatment for opioid use disorder (OUD), the medications used can be controlled substances with potential for misuse.
It’s important to be aware of these risks and use opioids responsibly. If you or someone you know is struggling with opioid use, seeking professional help is crucial.
Who is at Risk of an Opioid Overdose?
While anyone who uses opioids is at risk of an overdose, certain factors can significantly increase this risk. These include:
- Using Illegal Opioids: The use of non-prescribed, illicit opioids carries a high risk of overdose.
- Exceeding Prescribed Dosages: Taking more opioids than prescribed can lead to an overdose.
- Mixing Substances: Combining opioids with other medications or alcohol heightens the risk of overdose.
- Pre-existing Medical Conditions: Conditions like sleep apnea, or compromised kidney or liver function, can increase the likelihood of an opioid overdose.
- Age Factors: Individuals over the age of 65 are at a higher risk of experiencing an opioid overdose.
Being aware of these risk factors is crucial for preventing opioid overdoses. If you or someone you know falls into these risk categories, it’s important to exercise caution and seek guidance from healthcare professionals.
Prevention of Opioid Overdose
To effectively prevent opioid overdoses, specific measures need to be implemented alongside broader strategies to reduce drug use in communities. These measures include:
- Expanding Opioid Dependence Treatment: This involves increasing access to treatment for those dependent on opioids, including prescription opioids.
- Rationalizing Opioid Prescribing: Efforts should be made to reduce and prevent irrational or inappropriate prescribing of opioids.
- Monitoring Prescriptions: Keeping a close watch on opioid prescribing and dispensing practices.
- Regulating Over-the-Counter Sales: Limiting the inappropriate sale of opioids over the counter.
Despite these recommendations, there’s a notable gap in their implementation. Currently, only about half of the countries worldwide provide access to effective opioid dependence treatments. Moreover, less than 10% of people globally who need such treatment are actually receiving it, highlighting a significant area for improvement in addressing the opioid crisis.

Treating Opioid Overdose
In the event of a suspected opioid overdose, taking swift action can be life-saving. Here’s what to do:
- Call 911 Immediately: Quick emergency response is crucial.
- Administer CPR: If the person has stopped breathing or is breathing weakly, start CPR immediately, preferably if you’re trained in it.
- Use Naloxone: If naloxone is available, administer it to counteract the overdose. Naloxone is an FDA-approved medication specifically for reversing opioid overdoses.
It’s vital for family members, caregivers, and anyone frequently around individuals using opioids to recognize the signs of an overdose and know how to provide essential aid until professional medical help arrives. Remember, a person experiencing an opioid overdose cannot self-administer treatment. Being knowledgeable about naloxone, including how to obtain and use it, is an important part of preparedness. Consult with your healthcare provider for guidance on accessing naloxone in your area and for further information on managing overdose situations.
Opioid Overdose Treatment at Hope Harbor Wellness
Located in the serene suburbs of Atlanta, Hope Harbor Wellness is your ally in the fight against opioid addiction in Atlanta. Our drug rehab centers, dedicated to holistic recovery, are ideally situated to offer you the support you need.
Our compassionate outpatient program collaborates with top-tier medical opioid detox facilities, ensuring a safe and effective detox process. Once free from addictive substances, you can seamlessly transition into one of our specialized outpatient treatment programs at Hope Harbor Wellness, designed to address substance use disorders:
- Outpatient Rehab: A flexible program tailored to fit into your daily life.
- PHP (Partial Hospitalization Program): Offers a structured yet non-residential approach to treatment.
- IOP (Intensive Outpatient Program): Provides more intensive care while allowing you to maintain daily responsibilities.
- Dual Diagnosis Treatment Program: Caters to those with co-occurring mental health disorders.
Our opioid treatment programs incorporate a variety of interventions:
- MAT (Medication-Assisted Treatment): Utilizes medications to ease withdrawal symptoms and cravings.
- Psychotherapy: Addresses underlying psychological aspects of addiction.
- Group Therapy: Offers peer support and shared learning experiences.
- Individual Counseling: Provides personalized guidance and support.
- Family Therapy: Helps heal and strengthen family relationships.
- Holistic Therapies: Focuses on overall well-being, including physical, emotional, and spiritual health.
- Aftercare: Ensures ongoing support post-treatment.
Embark on your journey from addiction to recovery with Hope Harbor Wellness. Trust in our dedicated team to guide you every step of the way. For more information or to start your journey, call our admissions team at 678-929-6304.